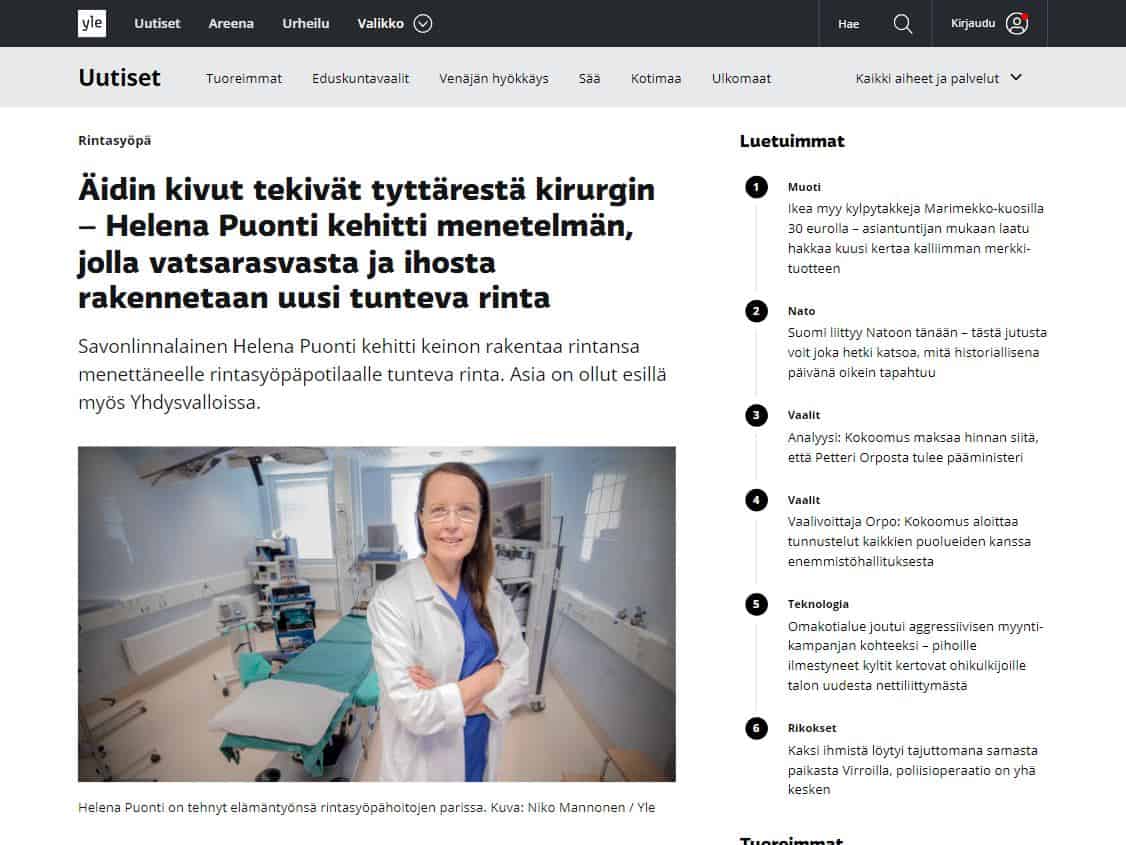
Helena Puonti
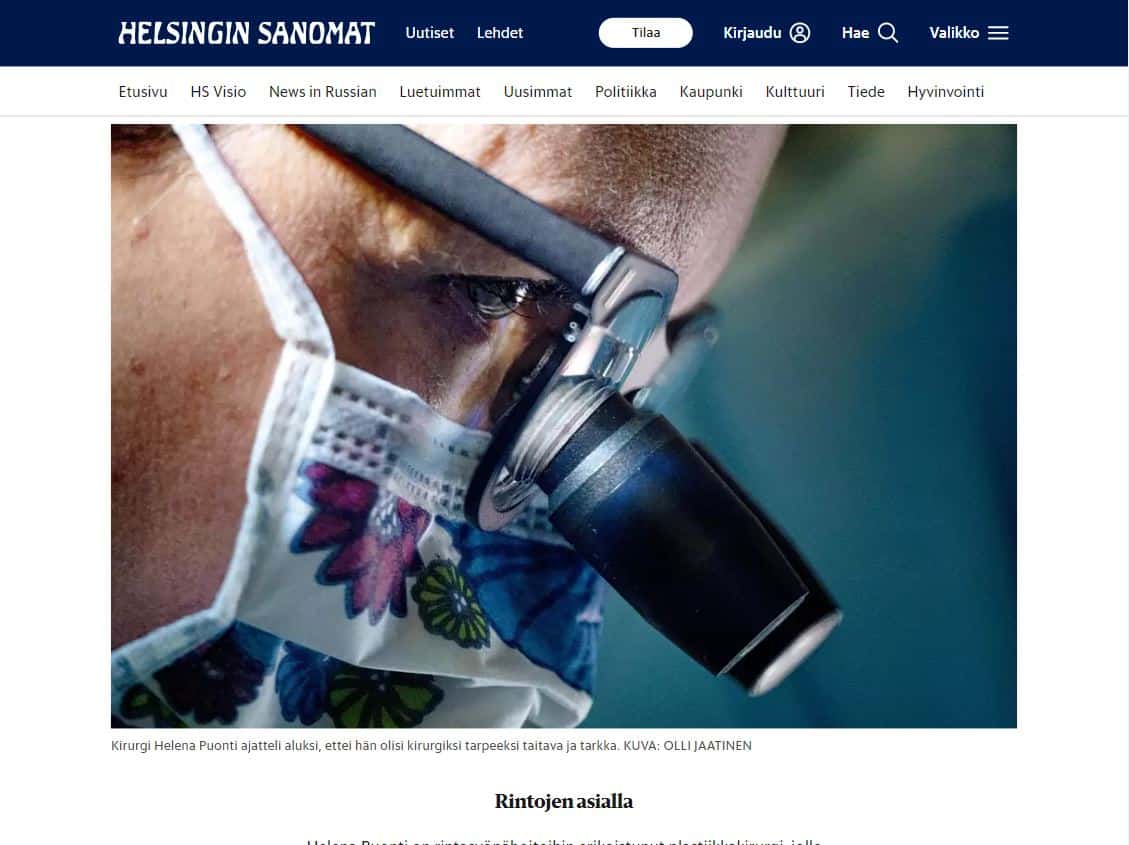
Helena Puonti on kansainvälisesti tunnustettu suomalainen plastiikkakirurgi ja rintasyöpähoitoihin erikoistunut mikrokirurgi. Helena on jo vuodesta 2001 saakka kehittänyt maailmanlaajuisesti ainutlaatuista mikroneurovaskulaarista “Tunteva rinta” -menetelmää, jonka ansiosta uudelleen rakennettuun rintaan on mahdollista palauttaa myös tunto.

Maailmanluokan osaamista ja Tunteva rinta
Monet Clinic Helenan potilaista tulevat klinikalle rintasyöpähoitoon Helena Puontin leikattavaksi, koska hän pyrkii käyttämään rintaa säästävää leikkausmenetelmää aina kun se on mahdollista.
Usein potilaat hakeutuvat rintarekonstruktioon saadakseen uuteen rintaansa kauniin ulkonäön lisäksi myös tunnon.
Helena Puonti on osoittanut, että luonnollinen tunto rinnan ihoon on mahdollista palauttaa jopa yhdellä vatsakielekkeen hermolla, kahdella hermolla tunnon palautuminen vahvistuu vielä enemmän.
Helena Puonti julkaisi tutkimuksensa väitöskirjassaan vuonna 2017.
Minun tarinani
Lääkärikoulun kävin Turussa. Kirurgian kurssin aikana totesin, että potilaan sairauden leikkaaminen ja haavojen hoitaminen on sitä perinteistä lääkärin työtä, johon olin aina halunnut.
Kirurgi tarvitsee paitsi hyvää käsityötaitoa, potilaan kuuntelemista ja ymmärtämistä sekä tietoa ja kokemusta. Tähän olen matkan varrella saanut oppia monelta hyvältä opettajalta.
Aloitin kirurgin työn Malmin aluesairaalassa Pietarsaaressa ensin apulaislääkärinä ja sittemmin osastonlääkärinä. Pietarsaaresta käsin suoritin kirurgian erikoistumisopintoni Keski-Pohjanmaan keskussairaalassa Kokkolassa sekä Tampereen yliopistollisessa sairaalassa. Valmistuttuani kirurgiksi muutin Savonlinnaan perhesyistä.
Savonlinna
Rintasyövän hoidon kehittymisen myötä kiinnostuin plastiikkakirurgiasta ja valmistuin plastiikkakirurgiksi kesällä 1998. Savonlinnan keskussairaala tarjosi minulle hyvät puitteet ja resurssit tehdä kaikkea sitä, mitä olin oppinut. Työsidonnaisuus alkoi kuitenkin käydä liialliseksi, niin että vähitellen siirsin työaikaani lisää yksityispuolelle.
Aloitin työn mikrokirurgian parilla vuonna 1991, valmistuin plastiikkakirurgiksi vuonna 1998 ja vuonna 2001 rakensin ensimmäisen tuntevan rinnan rintasyöpäpotilaalle yhdistämällä hermotuksen vapaakieleketekniikkaan.
Väittelin aiheesta tohtoriksi vuonna 2017, tutkimukseeni osallistui noin 100 potilasta, joille rakensin rinnan mikroneurovaskulaarisen TRAM kielekkeen avulla.
Tutkimukseni mukaan, palautunut tunto (kosketus, kuuma ja kylmä, kipu) oli keskimäärin 60% normaalin rinnan tunnosta, joskin mukana oli myös rintoja, joihin tunto palautui täysin.
Plastiikkakirurgia Helena Oy perustettiin joulukuussa 1999. Se on antanut meille väljemmät puitteet kehittää esteettistä kirurgiaa ja modernia rintasyövän hoitoa yksityisesti koko Suomen alueelle ja laajentaa asiakaskuntaa myös ulkomaalaisiin potilaisiin.
Esteettinen plastiikkakirurgia on erittäin haasteellista. Ei ole mitään standardileikkausta, vaan jokaisen potilaan kohdalla tulisi löytää ydinongelma ja ymmärtää potilaan toiveet.
Suurin osa esteettisen kirurgian koulutuksesta on täytynyt hakea ulkomailta. Leikkaamiseen liittyi aluksi paljon stressiä, mutta tieto ja kokemus tässä tapauksessa vähentää tuskaa ja antaa rohkeutta.
Sairaanhoitaja Päivi Tuominen toimii Clinic Helenan vastaavana hoitajana. Päivillä on yli 30 -vuoden kokemus hoitoalalta ja hänen tietotaitonsa ja ystävällisyytensä mahdollistaa, että potilaat saavat kysyessään leikkauksista etukäteistietoa ja leikkauksen jälkeen parasta mahdollista hoitoa yksikössämme.
Hyvässä työympäristössä ja työilmapiirissä on ilo hoitaa asiakkaita.
Tampere
Maaliskuussa 2022 laajensimme toimintaamme Tampereelle. Uusi rautatieaseman vieressä sijaitseva toimipisteemme parantaa saavutettavuutta ja antaa vaihtoehdon julkisen terveydenhuollon rinnalle, erityisesti rintasyövän hoidossa.
Tampereen toimipisteellämme voimme hoitaa leikkaukset joustavasti ja oma henkilökuntamme tarjoaa yksilöllistä hoitoa sisäänkirjautumisesta kotiutukseen asti.
Helsinki
Vastaanotolle on mahdollista päästä myös Helsingissä. Olemme aloittaneet vastaanotot Silutetti sairaalassa, aivan Helsingin keskustassa. Tavoitteena tuoda kaikkien saataville haastavat rintarekonstruktiot, kuten Tunteva rinta -menetelmä sekä vaativat leikkaukset kuten endoskoopinen implanttien laitto.
Palkintoja
Savonlinnan alueen tiedotusvälineet – 2016
Savonlinnan alueen tiedotusvälineet palkitsivat Helenan vuoden 2016 ansioituneena savonlinnalaisena.
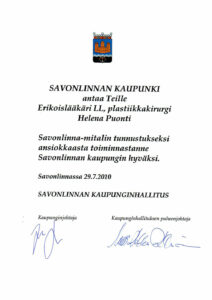
Savonlinnan kaupunki- 2010
Vuonna 2010 Savonlinnan kaupunki luovutti Helena Puontille Savonlinna mitalin tunnustukseksi ansiokkaasta toiminnasta kaupungin hyväksi.
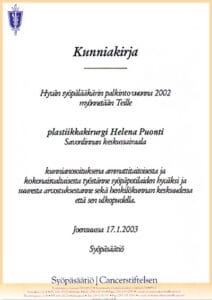
Syöpäsäätiö – 2002
Syöpäsäätiö palkitsi Helena Puontin “Hyvän syöpälääkärin” palkinnolla vuonna 2002 kunnianosoituksena ammattitaitoisesta ja kokonaisvaltaisesta työstä syöpäpotilaiden hyväksi.
Vuoden Rosina – 2001
Savonlinnan seudun liike- ja virkanaiset nimesivät Helenan vuoden Rosinaksi vuonna 2001 tunnustuksena hänen työstään talousalueen hyväksi.
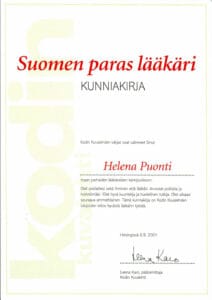
Kodin kuvalehti – 2001
Kodin Kuvalehden lukijat valitsivat Helena Puontin Suomen parhaiden lääkäreiden kärkijoukkoon vuonna 2001 kiitoksena hyvästä lääkärin työstä.
Julkaisut, Helena Puonti
- Helena K. Puonti, Satu K. Jääskeläinen, Helena K. Hallikainen, Taina A. Partanen. A new approach to microneurovascular TRAM-flap breast reconstruction, a pilot study. Journal of Plastic, Reconstructive & Aesthetic Surgery, 64, 346e352, 2011
- Helena K. Puonti, Satu K. Jääskeläinen, Helena K. Hallikainen, Taina A. Partanen. A Microneurovascular TRAM Flap Does Not Compromise Abdominal Sensibility More Than a Conventional One. Plast Reconstr Surg 130(3):382c, 2012
- Helena K. Puonti, Satu K. Jääskeläinen, Helena K. Hallikainen, Taina A. Partanen. Improved sensory recovery with a novel dual neurorrhaphy technique for breast reconstruction with muscle-sparing TRAM flap technique. Microsurgery, 37 (1) 21-28, 2017
- Helena K. Puonti, Taina A. Broth, Seppo O. Soinila, Helena K. Hallikainen, Satu K. Jääskeläinen. How to assess sensory recovery after breast reconstruction surgery, Clinical Breast Cancer, 17 (6): 471-485, October 2017
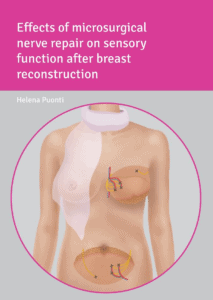
- Helena K. Puonti: Dissertation, Effects of microsurgical nerve repair on sensory function after breast reconstruction. Helsinki University, 27.01.2017
Väitöskirja, Helena Puonti
Helsingin yliopisto, lääketieteellinen tiedekunta, 27.01.2017
Effects of microsurgical nerve repair on sensory function after breast reconstruction
Lähes 40 % rintasyöpäpotilaista menettää rinnan rintasyöpäleikkauksessa. Plastiikkakirurgiajohtoinen rintasyövän hoito Suomessa on mahdollistanut rinnan muodon palauttamisen potilaille tarvittaessa osana normaalia rintasyövän hoitoprosessia.
Vapaalla vatsakielekkeellä saadaan rekonstruoitua luonnollinen ja kaunis rinta, mutta sen haittapuolena on rakennetun rinnan huono tunto. Lue lisää Tuntevasta rinnasta täältä.